What the data says
Laudio’s recent analysis of a national dataset of 150+ hospitals identified eight key predictors of RN burnout, detailed below. Additional analysis determined the nurse-level and department-level thresholds at which each of these eight metrics become predictors of elevated risk of burnout and turnover and the team level.
The eight burnout predictors - selected based on a combination of reasons, including peer-reviewed research on role overload and role conflict and the ability of most health systems to measure them - are proposed as an “early warning system” for healthcare leaders and broken down in An Early Warning System for Nurse Burnout: Metrics and Strategies, a fall 2025 joint report from Laudio and the American Organization for Nursing Leadership (AONL).
The eight RN burnout predictors are:
|
Role overload indicators |
Role conflict indicators |
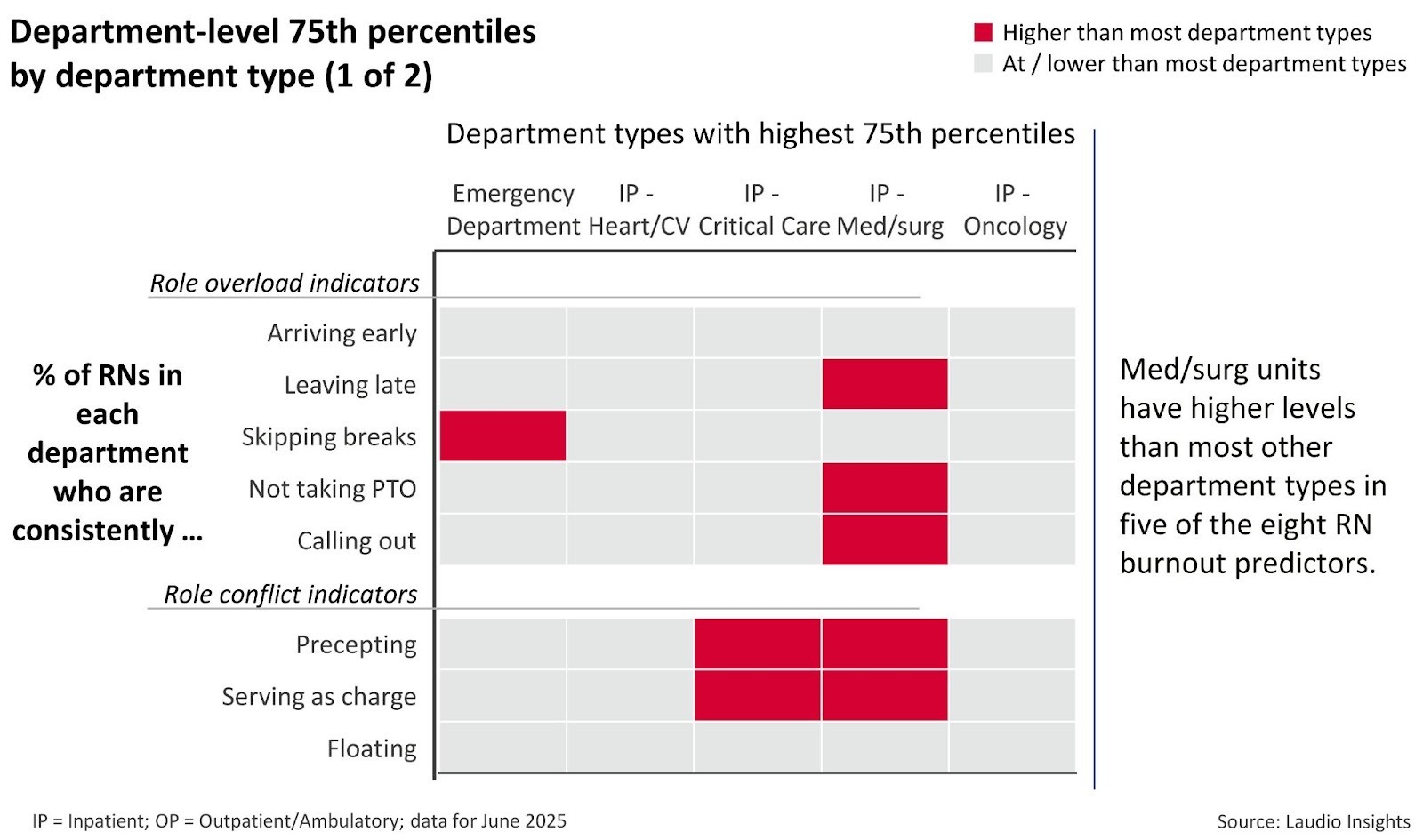
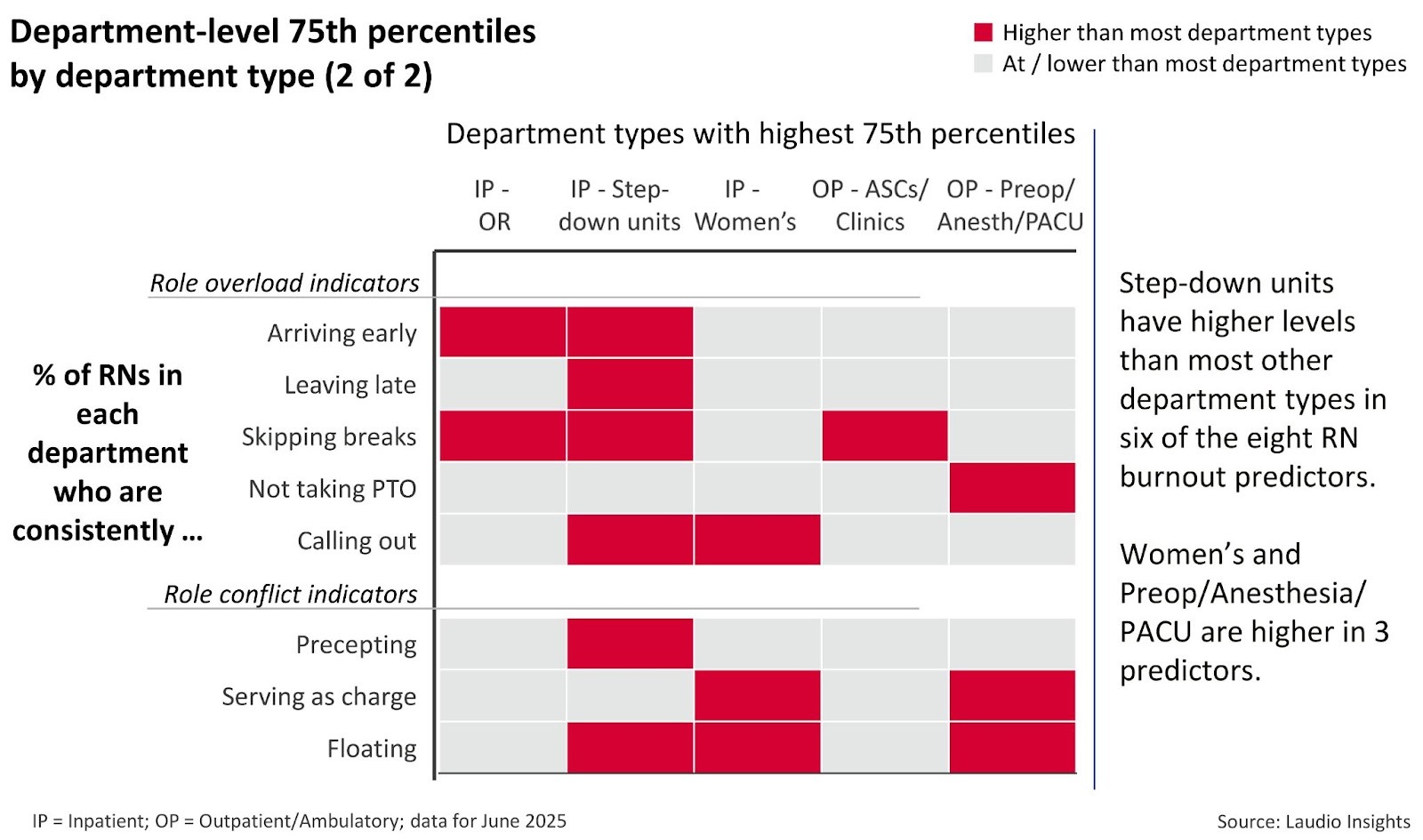
The two charts below show which of ten different department types have substantially higher than average levels for each of the eight predictors. The burnout predictors’ prevalence differs across department types. For example, emergency departments (EDs) see a much higher rate of RNs regularly skipping breaks, as shown in the first column of the first chart. Across all ten departments included in the report, Step-down units and med/surg have the highest number of elevated rates of the key burnout predictors.
What it means
Patterns vary by department, but leaders shouldn’t accept them as inevitable
Across all service lines, interviews with RNs and managers consistently emphasized leadership practice and cultural norms that can influence operational conditions. Skipping breaks and regularly leaving late cannot be normalized, and excessive floating becomes unsustainable when it leads to role stress or compromises a healthy work environment. By integrating technology to ensure these metrics - which are predictive of burnout - are visible to executive and frontline leaders, unhealthy workplace practices can be proactively addressed before they are normalized.
Implications for healthcare managers
Managers should aim to partner with their executives to identify proactive strategies to address any present burnout predictors within their department. As one executive said, when interviewed about these topics, “it is not a single person’s responsibility to create a team’s ability to thrive.”
From both a manager and executive perspective, specific potential tactics to address them include:
Managers: Leverage the team around you
-
- Given wide spans of control, managers cannot carry this responsibility alone. Engaging assistant nurse managers, educators, coordinators, preceptors, and team leaders as extensions of leadership helps track risks and provide real-time support.
- When these roles are fully integrated, managers create a coordinated leadership structure. This shared accountability strengthens early intervention and reduces burnout.
- Many of these activities involve building a “team of teams”. Additional quick wins on this topic are provided in Leader Inspired Work, a Laudio Insights publication written for and by healthcare managers.
- Given wide spans of control, managers cannot carry this responsibility alone. Engaging assistant nurse managers, educators, coordinators, preceptors, and team leaders as extensions of leadership helps track risks and provide real-time support.
Executives: Build for visibility
-
- Pinpointing burnout risks depends on clear access to operational signals, such as patterns in overtime, time-off usage, and after-hours work.
- It also relies on understanding workplace norms: how leaders support well-being, recognize individual needs, and uphold healthy boundaries. All of these broaden the ability to evaluate and address burnout effectively.
- Pinpointing burnout risks depends on clear access to operational signals, such as patterns in overtime, time-off usage, and after-hours work.
Because these predictors surface in daily work patterns, leaders need resources to help them identify and act on them early before they manifest as burnout or turnover. For more insights on the metrics and proactive strategies to prevent RN burnout, access An Early Warning System for Nurse Burnout: Metrics and Strategies.
Written by Tim Darling
Tim Darling is a co-founder and President, Laudio Insights. With over 20 years of experience in healthcare technology, Tim has a real passion for using data and analytics to serve the challenges facing healthcare organizations. Prior to Laudio, Tim was on the leadership team of a healthcare education analytics company and he spent seven years as a consultant at McKinsey & Company. He has an MBA from Carnegie Mellon and BS degrees in Mathematics and Computer Science from the University of Maryland, College Park.
